Why is it so important to have a company policy that also covers the topic of mental health? First, one in three employees (1 in 3!) has or will be affected by a mental health issue. Secondly, the prevalence of mental disorders is on the rise in industrialized countries and has become a priority in developing countries: according to the WHO, psychosocial risks and the risk of work-related stress should be included as a first priority in the policy and research agendas of developing countries.
Mental health problems and other stress-related disorders are recognized as being among the main causes of early retirement, high absenteeism rates, general health problems and poor organizational efficiency. In addition, mental health risks are also linked to new technologies, digitization, the information avalanche, or over-information (infobesity as Canadians say). And we have not even started talking about the arrival of COVID which suddenly brought out more mental disorders than previously, and a ‘new normal’ to which we need to adapt. Do we need more reasons to convince organisations to tackle this topic as part of their corporate health strategy?
What do we mean by mental health?
It is the capacity that each of us has to feel, think and act in ways that improve our ability to enjoy life and meet the challenges we face. It is a positive sense of emotional and spiritual well-being that incorporates culture, equity, social justice, interactions, and personal dignity.
Mental health is somewhat the opposite of mental illness, also less stigmatically referred to as mental disorder. Mental illness is characterized by alterations in thinking, of the mood or behaviour (or a combination of the three) associated with distress and marked dysfunction.
Yes, also and especially in business, it is important to talk about mental disorders, to stop the stigmatization and allow everyone to be offered a diverse and inclusive environment. Providing an inclusive and non-stigmatizing professional environment is therefore crucial for these employees.
But first, let’s redefine the terms, so that we’re all talking about the same thing.
Many terms are used to designate mental disorders: in addition to mental illness, we also hear the expressions mental disorder, mental crisis, psychiatric illness, nervous exhaustion or even burnout. Familiar expressions – like the one I heard not even an hour ago in the mouth of my dear partner – such as bonkers, mentally ill, mad, crazy, crippled, or deranged promote rejection and should not be used, especially since these in no way convey what the people concerned are going through (ensa, 2020). In business, the term mental health, or mental disorder, does not have a good press. Indeed, we often wrongly associate the word “mental” and “disabled”. Yes, yes, I promise you, I heard it in a large Swiss company.
The term mental disorder is therefore a broad term encompassing both mental illnesses and their symptoms, which may not be severe enough to allow a pathology to be diagnosed, while also including crisis states associated with a mental illness (ensa, 2020). Subsequently, we will use the term mental disorder which we find much more appropriate than all the others and which we recommend using to avoid any discrimination.
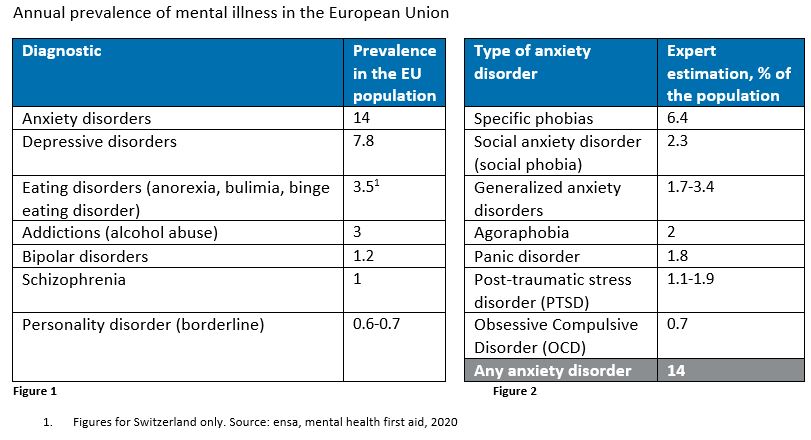
Let me take a break here to explain in a simple way the mental disorders that exist in the world, and therefore also within any organization. If you are aware of this type of disorder, I will let you skip to the next part. Here they are listed, in order of importance according to the number of people suffering from these mental disorders in Europe.
Anxiety Disorders:
The most common forms of anxiety are phobias, panic disorder, and generalized anxiety disorder. See Figure 2 below for a summary of the prevalence of anxiety disorders in the European Union.
Severe and persistent depression:
Depression is a psychosomatic disease (it associates psychic and somatic symptoms – relating to the body) due to an imbalance in mood. Mood is defined as the affective and emotional disposition that conditions the way in which we experience events that normally generate joy or sadness. The mood disorder no longer allows these normal alternations of joy and sadness. The disease will affect memory, thinking, judgment and the state of mind. It has an impact on the way you feel, think, sleep and act. Unlike transient depressions caused by life’s sorrows, the person will not be able to overcome this deep feeling of sadness on their own.
Eating Disorders:
These disorders appear in adolescence, affect women more often than men and include anorexia nervosa (dietary restriction, fear of gaining weight, altered perception of body shape), bulimia nervosa (eating a large amount of food over a limited period of time, followed by compensatory behaviours such as vomiting, taking laxatives, fasting, or excessive exercise) and binge eating disorder (bulimia without compensatory behaviour and which causes overweight and generates psychic suffering).
Addictive disorders or addictions:
We talk about physical or psychological dependence when a person is no longer able to function without consuming a given substance. These disorders include alcoholism and smoking (legal drugs), drug abuse and diversion, drug addiction (illegal drugs: ecstasy, cannabis, cocaine, amphetamines, hallucinogens, opioids) and behavioural addictions (gambling, gaming, sex, compulsive shopping, social media, etc.).
Bipolar disorder or manic depression:
This disorder is usually diagnosed in adulthood and has two poles of emotion. These are recurrent, abnormal, persistent, and uncontrollable mood swings, alternating phases of hyperactivity during which a feeling of super-power dominates, followed by severe phases of depression. The resulting emotional chaos can have serious consequences especially from a social point of view.
Schizophrenia:
Contrary to popular belief, the term ‘schizophrenia’ does not mean ‘double personality’, it comes from the Greek and means ‘fragmented mind’. It is a mental illness that usually begins between the ages of 15 and 30, and is accompanied by loss of contact with reality, delusions, hallucinations, changes in thought, language, and behaviour. People are often unable to distinguish between reality and their own perception of events. This disease affects about 1% of the population.
Personality Disorder:
This disorder affects about 0.7% of the population, more women than men, and occurs in early adulthood. It is a disorder that refers to psychological and social dysfunction. The person has maladaptive and entrenched behaviours. His/her personality is abnormal, either in the balance of his/her judgment, emotions, and his/her behaviours. His/her relationships with others are often very unstable.
How to approach this topic within an organisation?
-
By providing a culture that embraces diversity and inclusion.
It is about putting an end to the stigma, by raising awareness on the subject to break the silence and the taboos on mental disorders. This is exactly what one of my clients did recently: using the needs and risks analysis I completed, they created a new Health & Resilience department reporting to the Inclusion & Diversity (I&D) department. In order to address mental disorders and ensure better mental health for your employees, you have to talk about inclusion, differences, taboos, stigma, and there is no better department than I&D to cover such topics.
-
By setting up a health policy including a pillar focused on mental disorders and psychosocial risks.
See our article on stress, psychosocial risks to assist you in the process.
-
By promoting specific programs and workshops to better understand the subject:
first aid in mental health (by ensa), mentoring, stress/anxiety/addictions management, employee assistance program (EAP), etc.


