Reduced for a long time to the simple notion of stress, psychosocial risks (PSR) have become a major concern of health and wellbeing at work, and organizations try to deal with them often too clumsily. Indeed, the effects of mental health disorders in the corporate world have never been greater or more visible than now. The latest WHO report (2019) shows that the global economy loses an average of US $ 1 trillion (yes with 12 zeros: 1,000,000,000,000) each year due to lost productivity due to depression or anxiety. So, what do organisations do?
I can hear you telling me, rightly so, that not all companies have the internal resources to successfully identify psychosocial risks. But are we asking the right question here, is it really a question of resources? Or are the recommended methodologies and analysis tools simply not adequate to meet the needs of small, medium, and large structures? But let’s not get carried away and let’s start from the beginning, namely, what is PSR?
Are psychosocial risks singular or plural?
Psychosocial risk is defined, according to the European Agency for Safety and Health at Work, as the risk of harming the psychological or physical wellbeing of a worker arising from poor work design, organisation and management, as well as a poor social context of work. Psychosocial risks are much more complex and more difficult to manage than traditional risks for health and safety at work such as industrial hygiene, ergonomics, etc. Indeed, even the most specialised organizations working on the this subject, whether it is the WHO, the International Labour Organization (ILO) or the European Agency for Health and Safety, the identification or definition of risks differ, and that’s not to mention strategies to reduce them.
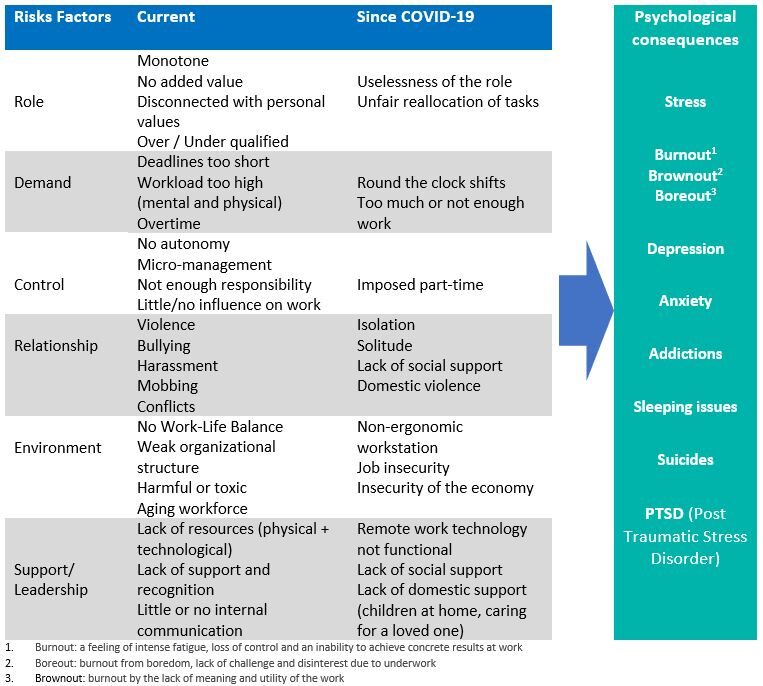
Let me summarise below what I found during my research. Here is a list of psychosocial risk factors, which result from a poor design, organisation or management of work and an unfavourable socio-professional context. In addition, I have also listed new examples that have emerged with the arrival of the pandemic due to COVID-19. On this subject and as a bonus, I found this new guide that the ILO published in summer 2020 to help employers put in place preventative measures to protect the health and wellbeing of employees in the context of the pandemic. I thought you might find it handy.
I also thought it would be useful to add to the list the main psychological consequences that will have an impact, direct and indirect, on your costs. I have deliberately ignored the physical consequences such as musculoskeletal disorders, cardiovascular disease, diabetes, etc. which can also arise from psychosocial risks, but which are not the subject of this article.
How to reduce these risks?
When you see the length of the list of risks, which has nearly doubled since the arrival of COVID-19, I understand if HR managers might start hyperventilating. Nevertheless, it is worth highlighting – and not only to protect HR managers’ health – that it is not up to organisations to alleviate all psychosocial risks, but the main ones, or at least those that make the most sense in your organisation.
As with many interventions related to health and wellbeing at work, there are key prerequisites to implement a successful psychosocial risk reduction strategy:
- The visible and personal commitment of each member of your management committee
- Voluntary participation of employees during risk analysis
- Open communication and regular consultation between management and employees
- Values of your organization aligned with the wellbeing of your employees
Here are four steps that will help you reduce PSR, including the first one which I will call Major Step. If you don’t start with this one, don’t bother with the others.
Major Step: Perform a risk analysis, with the right tool
This step is essential for a good understanding of the situation, and the Health Risk Assessment (HRA) is essential for a holistic analysis of your health risks, including psychosocial risks. Yes I am a massive fan of such tools, which are scientifically validated, confidential, anonymous, 100% online, allowing total automation of the collection of information as well as of the restitution of results, easy to use and require very few resources.
The HRA differs from classic risk analysis tools commonly used by Safety Managers and based on a risk management method. Such type of tool has proven its worth in the past, and is still strongly promoted today by renowned institutes such as INRS (National Institute for Research and Safety) in France which uses the RPS-DU tool, or the European Agency for Safety and Health at Work (EU-OSHA) which uses the ESENER tool. Several years of attempts to make these tools compatible with health or psychosocial risks analysis have not really been successful. This is because they are very often complicated, difficult to use, they take a long time to set up and require the presence of several experts. In today’s world, and even more since COVID-19, we need to find more agile tools, easy to use remotely, automated, and much more responsive. Indeed, the use of an online HRA will allow you to collect anonymously and extremely quickly, the following information, essential to better understand your psychosocial risks:
- Work Stressors (lack of autonomy, lack of recognition)
- Job satisfaction factors (effort and demand)
- Organizational modifiers including respect, fairness, support from manager
- Sleep and fatigue
- Depression
- Reason for stress: related to professional life, private life, personality
- The HRA also measures – confidentially and anonymously – all aspects of health related to nutrition, physical activity or sedentary lifestyle, alcohol or tobacco consumption, weight, family status, biometric data (cholesterol, blood pressure), risks of chronic diseases and diabetes, restrictions on work, etc.
If you are interested in testing our HRA for free, you will find more information here (free demo).
Step 1: Develop a culture / environment conducive to health and well-being
The HRA used during the Major Step allow you to identify your needs: it is in a way the diagnosis of the soil on which you want to build.
Now it is time to shape your foundations. They must be directly linked to the health and wellbeing of your employees. Here is a non-exhaustive list of basic initiatives that will have an impact on the psychosocial risks of your organization:
- Policies & Regulations: on overtime, on vacation, on harassment, ethics and compliance, code of conduct, etc.
- Training: first aid in mental health, addictions, sleep and fatigue, resilience, stress and change management, psychosocial risks, suicide prevention especially in high-risk companies
- Resources: Person of trust, internal mediator, occupational health nurse, Employee Assistance Program
- Coaching / Mentoring
If you’re looking for inspiration on how to put together a health and wellness strategy to ‘healthily’ impact your corporate culture, read our 10-step model here.
Step 2: Encourage dialogue and listen to employees
As in a traditional risk analysis approach, the element of discussion, interviews, feedback, and other employee opinion polls is important to understand where the areas for improvement are and then be able to respond in a targeted way.
Step 3: Train and coach leaders
Several studies show a direct link between manager’s skills, behaviors and habits and mental health of their direct reports. Also, to ensure good mental health of his/her team members, a leader must be trained on how to detect health risks, including PSRs, and how to behave in a way that will help reduce such risk to improve health and wellbeing of his/her team. Such training should cover skills, knowledge, and behaviors such as respect, trust, communication, conflict management, accessibility, empathy, courage to name a few. They should also include leaders’ self-assessment, specific components on leaders’ selfcare, how to look after themselves, how to manage their own stress level as well as their emotions.
These steps 2 and 3 are the material to use for your building structure.
Where does employer’s responsibility begin and where does it end?
Do some of you still wonder whether it is your responsibility as an employer to find solutions for your employees’ mental health? Well yes, sorry to disappoint, it is the employer’s duty to find solutions for their employees’ physical and mental wellbeing. According to the European Agency for Safety and Health at Work, helping to manage stress is not only a moral obligation and a good investment for employers, it is also a legal obligation laid down in framework directive 89/391 / EEC.
And I still have not told you about the costs that PSRs generate. If you are still doubting the importance of acting upstream on psychosocial risks prevention, the below information should convince you.
And how much does it all cost?
There are several guidelines designed to help organizations better understand the estimated financial cost of psychosocial risks and stress at work.
Here is one of them, developed by Ravi Tangri, Canadian expert in strategy and leadership, and author of the book “Stress Costs, Stress Cures”. His formula which incorporates six elements is one of those presented by the European Agency for Safety and Health at Work:
| · 19% of absenteeism costs |
| · 40% of staff turnover costs |
| · 55% of Employee Assistance Program (EAP) |
| · 30% of short- and long-term disability costs |
| · 60% of total costs of workplace accidents (professional only) |
| · 100% costs of workers’ compensation and lawsuits due to stress |
A few years ago, I used this formula to calculate the annual costs related to stress and psychosocial risks for one of my clients. My client is a company based in Switzerland, with around 3,000 employees, well positioned on the market, with an average absenteeism rate (4%), below average employee turnover rate (3%), a classic EAP of less than CHF40/employee, short- and long-term disability costs and workplace accident costs of less than CHF1m, no costs related to workers’ compensation claims and stress-related legal proceedings. Despite this, the annual costs related to stress and PSRs reached CHF3.9 million. Scary isn’t it? Using Tangri’s formula helped convince my client to put a leadership program in place, including coaching, feedback, psychological safety, absence management, and empathy and courage components.
In conclusion, it is true that mental health and psychosocial risks in the workplace have been recognized as a priority in the European Union for at least two decades. However, it is not certain that the declared ambitions in this area have been achieved, mainly for two reasons:
- the relationship between mental health in the workplace and the importance of preventative actions still seems to be lacking.
- the methods and tools used and recommended do not encourage organisations to act upstream.
Finally, the management and especially the reduction of psychosocial risks are a major issue for organisations. When properly tackled, it shows an organisation’s ability to be efficient and sustainable. This subject is obviously dictated by questions of costs, productivity, and legal obligations. It is also a public health issue, since thanks to its ability to reach all active members of the labour market, the workplace is and must remain a fundamental player in the promotion of mental health in the population.